From Fragile to Resilient
Your Guide to Bone Health and Osteoporosis Awareness

[Toc]
A Silent Threat to Bone Health
Osteoporosis, a condition characterized by weakened and brittle bones, affects a staggering number of individuals. In the United States alone, an estimated 10 million people grapple with this silent disease, with women constituting a significant majority, comprising around 80% of those affected. The implications of osteoporosis are far-reaching, with the statistics revealing a startling reality.
A startling fact underscores the vulnerability of women as they age: approximately one in two women over the age of 50 will experience a bone fracture due to osteoporosis. In fact, the risk of breaking a hip for a woman equals the cumulative risk of facing breast, uterine, and ovarian cancer combined. The implications of osteoporosis extend beyond fractures; it has the potential to significantly impact the quality of life and independence of those affected.
It's vital to recognize the factors that influence an individual's susceptibility to osteoporosis. The bone density achieved prior to menopause serves as a foundation for future bone health. A higher initial bone density can translate to a reduced risk of developing osteoporosis later in life. Conversely, low peak bone mass or the presence of risk factors contributing to bone loss can elevate the likelihood of developing the condition.
Equally critical is the rate at which bone loss occurs following menopause. For some women, this loss can be accelerated, leading to the depletion of up to 20% of bone density within five to seven years following menopause. The speed of bone loss becomes a key determinant in the likelihood of developing osteoporosis.
In this intricate interplay of factors, the importance of understanding osteoporosis becomes evident. With its subtle onset and potentially severe consequences, empowering individuals with knowledge about risk factors, prevention, and management is paramount.
Osteoporosis leads to easy bone fractures, sometimes from a simple sneeze or cough. Even bumping into a table can lead to a fracture. It's also more challenging for your bones to recover after a fracture, often causing permanent pain and sometimes disability. Spine and hip fractures are especially grievous, as they may decrease quality of life.
The information below delves into the complexities of osteoporosis, offering insights into strategies that can fortify bone health, enabling individuals to lead active, fulfilling lives well beyond their prime.
Note: This post is intended for informational purposes only. For personalized guidance and healthcare recommendations, it's advisable to consult a qualified healthcare professional.

Understanding Osteoporosis: Fragile Foundations
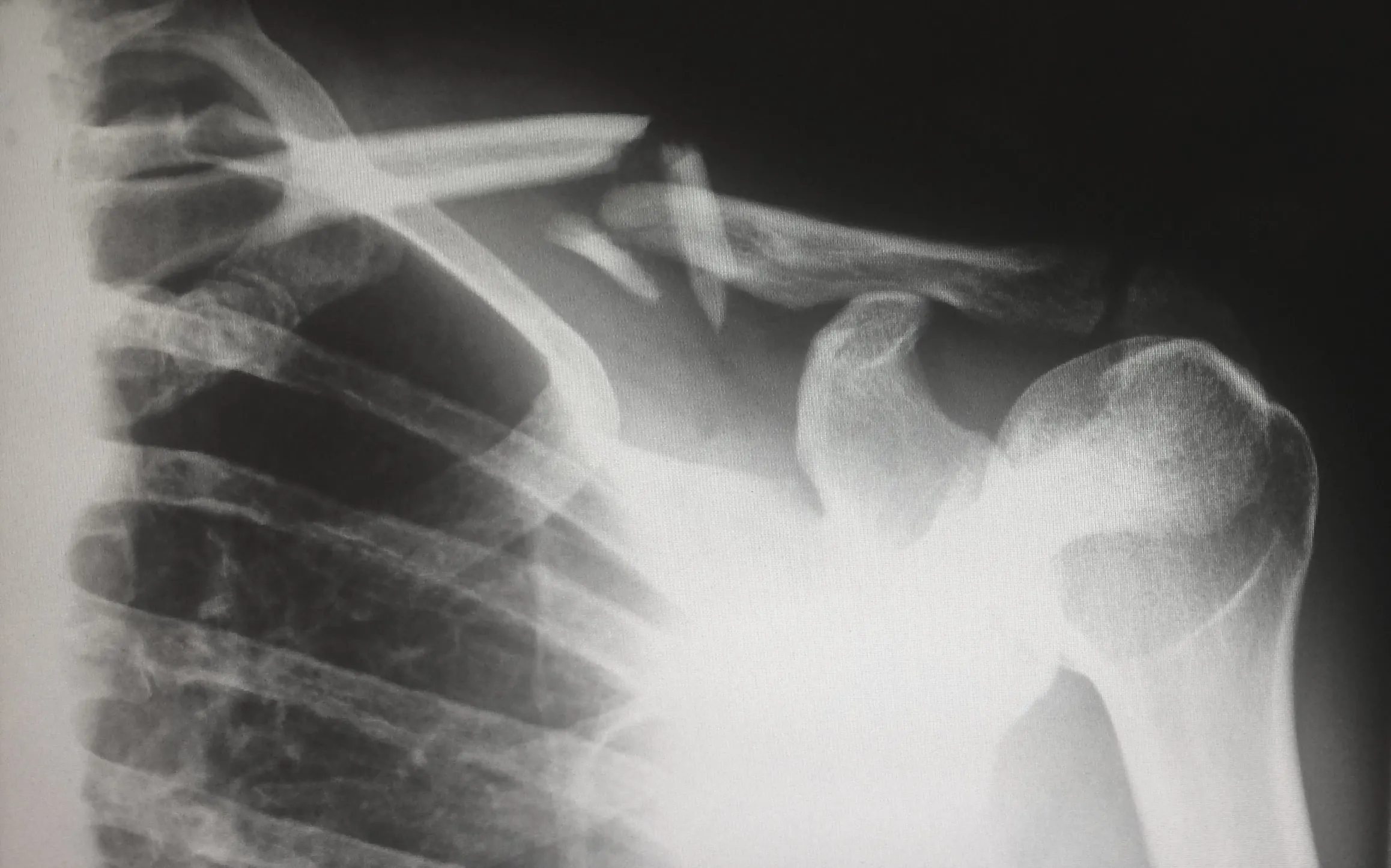
Imagine your bones as intricate structures, resembling the delicate pattern of a honeycomb. Just like a honeycomb provides structural integrity, your bones' internal architecture plays a pivotal role in maintaining strength. This structural lattice is the essence of bone health.
However, when osteoporosis takes hold, this once-sturdy framework undergoes a profound transformation. The normally inconspicuous spaces within this "honeycomb" structure begin to enlarge, rendering the bone notably weaker and more brittle. This weakening of the bone's internal structure marks a hallmark of osteoporosis, potentially setting the stage for fractures and a diminished quality of life.
As these changes occur beneath the surface, the urgency to comprehend and address osteoporosis becomes evident, illuminating the path toward preserving the resilience and vitality of our skeletal foundations.

Common Signs and Symptoms
Back Pain: Osteoporosis-related fractures, especially in the spine, can lead to chronic back pain.
Fractures: Bones become more fragile with osteoporosis, making them susceptible to fractures, even from minor bumps or falls. Common fracture sites include the wrist, hip, and spine.
Loss of Height: Compression fractures in the spine can cause a gradual loss of height over time.
Stooped Posture: Osteoporosis-related fractures in the spine can lead to a stooped or hunched posture known as kyphosis.
Weakness and Fatigue: Muscular weakness and fatigue may be experienced due to changes in posture and reduced physical activity to avoid pain.
Limited Mobility: Fractures and bone loss can impact mobility and the ability to perform daily activities.
Sudden or Severe Back Pain: In some cases, sudden or severe back pain could indicate a vertebral fracture, especially if there was no significant trauma.
It's important to note that these signs and symptoms can be caused by other conditions as well. If you suspect you may have osteoporosis or are at risk, it's advisable to consult a healthcare professional for proper evaluation, diagnosis, and management.

Importance of Bone Health
As women age, especially after reaching 45, their bodies undergo various changes, including hormonal shifts and decreased bone density. These changes can lead to an increased risk of osteoporosis and fractures.
Focusing on maintaining strong bones is crucial for ensuring a healthy and active lifestyle in later years. While Hormone Replacement Therapy (HRT) is a possible option for managing menopausal symptoms and bone health, this post will focus on natural methods to support bone health.
Cultural Variations and Bone Density in Women
Cultural differences can play a significant role in bone density variations among women. Traditional dietary habits and lifestyle practices unique to different cultures can influence bone health outcomes. For example, cultures with traditions involving weight-bearing activities, like farming or manual labor, can potentially enhance bone density.
However, modernization and sedentary lifestyles in some cultures might lead to decreased bone health. In the US alone…
- 20% of Caucasian women age 50 and older are estimated to have osteoporosis
- 5% of African American women and older are estimated to have osteoporosis
- 50% of Latinas older than 50 have low bone mass but don’t yet have osteoporosis
Recognizing the cultural aspects impacting bone health can guide tailored interventions. Encouraging diverse dietary options and blending traditional practices with modern exercise routines can contribute to healthier bones across different cultural backgrounds.
Other Factors Affecting Bone Health
Several other factors contribute to bone health, including hormonal changes, diet, lifestyle, and physical activity. Genetics plays a role in determining an individual's bone density potential, but lifestyle choices can significantly influence whether that potential is realized. Hormonal changes, particularly the decrease in estrogen during menopause, can lead to accelerated bone loss. This makes it even more important for women over 45 to take proactive measures to support their bone health.
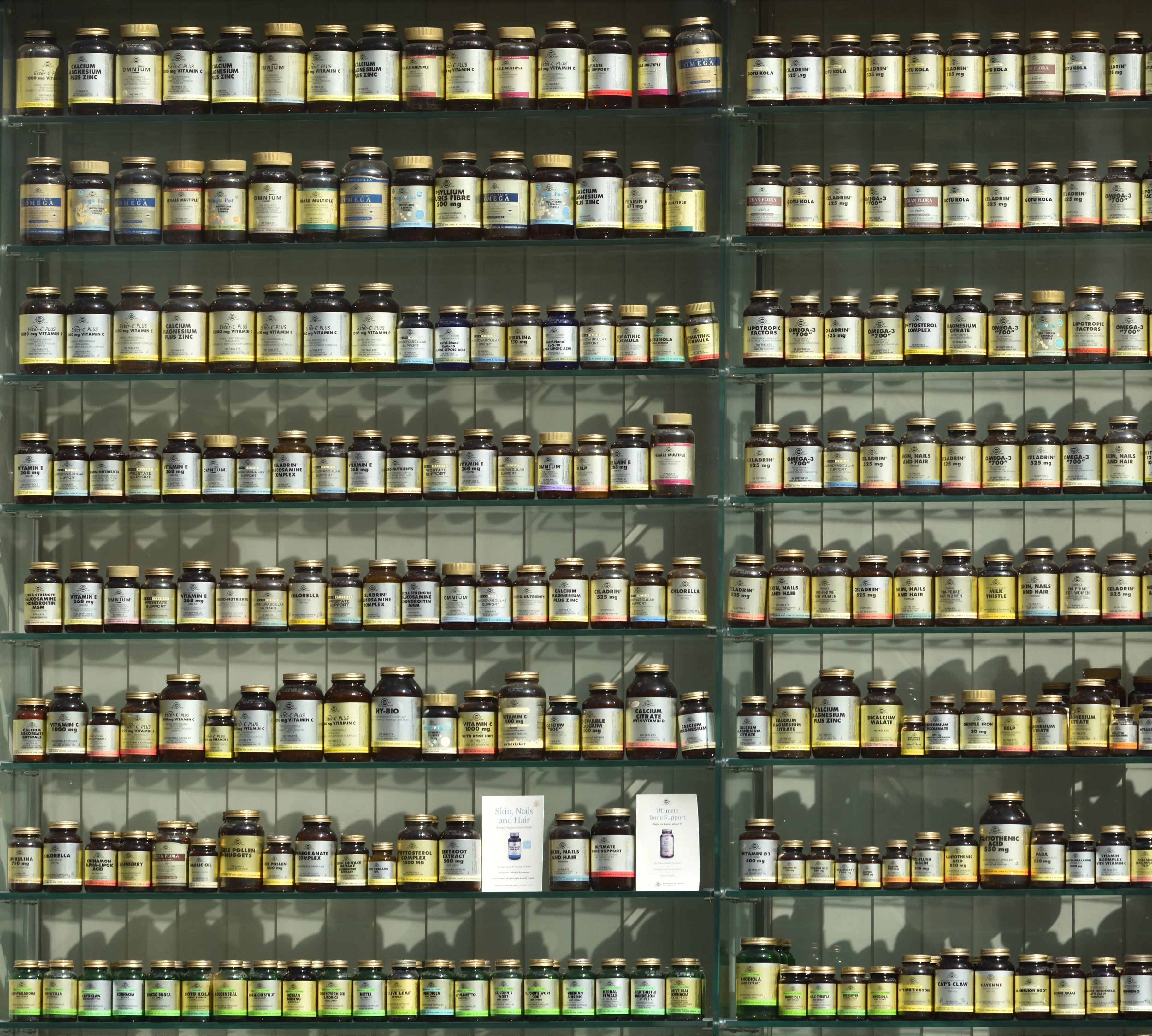
Vitamins and Minerals for Strong Bones
A balanced diet plays a role in maintaining bone health. Both calcium and magnesium are essential minerals for bone health, and both play distinct roles in maintaining strong and healthy bones.
Calcium
- Calcium is a major component of bone structure and provides the rigid framework that gives bones their strength.
- It is crucial for bone formation, growth, and remodeling throughout life.
- Adequate calcium intake helps prevent conditions like osteoporosis, which is characterized by brittle and weak bones.
- Dairy products, leafy greens, fortified foods, and supplements are common sources of calcium.
Magnesium
- Magnesium is also essential for bone health as it is involved in converting vitamin D into its active form, which is necessary for calcium absorption.
- Magnesium aids in regulating calcium levels in the body and helps maintain the proper balance between calcium and other minerals.
- It supports bone density and overall bone structure.
- Nuts, seeds, whole grains, leafy greens, and legumes are good sources of magnesium.
Magnesium not only contributes directly to bone health but is also responsible for orchestrating over 300 biochemical reactions within the body. These reactions are essential for various bodily functions that collectively support optimum health. While calcium certainly plays a pivotal role in bone structure, magnesium acts as a conductor, ensuring that calcium is appropriately utilized to maintain bone density.

Vitamin D
Vitamin D is essential for calcium absorption and can be obtained from sunlight exposure and fatty fish like salmon and mackerel. Incorporating these nutrient-rich foods into your daily meals can contribute to optimal bone health.
Women, especially those after menopause, may experience difficulties with vitamin D absorption due to several factors:
Hormones: hormonal changes, such as a decrease in estrogen levels, can affect the body's ability to absorb and utilize vitamin D efficiently. Estrogen plays a role in maintaining bone health and aiding in calcium absorption, which is closely linked to vitamin D metabolism.
Age-related Changes: With age, the skin's ability to produce vitamin D upon exposure to sunlight decreases. This is significant because the primary natural source of vitamin D is through synthesis in the skin when it's exposed to UVB sunlight. As people age, their skin becomes less efficient at producing vitamin D.
Decreased Sunlight Exposure: Adequate sunlight exposure is crucial for the body's production of vitamin D. The combination of age-related changes and decreased outdoor activity can lead to lower vitamin D levels. Experts suggest a range of 10–30 minutes of sun exposure, particularly between 10 am and 4 pm, at least twice a week, to the face, arms, hands, and legs without sunscreen is enough to produce adequate levels of vitamin D in the body.
Reduced Dietary Intake: Postmenopausal women might also experience changes in dietary habits, which can affect their vitamin D intake. Foods rich in vitamin D, such as fatty fish, fortified dairy products, and egg yolks, might not be consumed as frequently as needed to maintain optimal vitamin D levels.
Gut Health and Absorption: As people age, digestive functions can change. Some postmenopausal women might experience decreased efficiency in absorbing nutrients from the gastrointestinal tract. This can impact the absorption of fat-soluble vitamins like vitamin D.
Obesity: Obesity is associated with reduced bioavailability of vitamin D. Postmenopausal women who are overweight or obese might have a higher risk of vitamin D deficiency due to the sequestration of vitamin D in adipose tissue.
Medical Conditions and Medications: Certain medical conditions that become more prevalent with age, such as Crohn's disease, celiac disease, and kidney problems, can affect the body's ability to absorb and utilize vitamin D. Additionally, some medications, like certain anticonvulsants and glucocorticoids, can interfere with vitamin D metabolism.
It's important for postmenopausal women to monitor their vitamin D levels and consult with healthcare professionals if they suspect a deficiency. In some cases, vitamin and mineral supplements might be recommended to help maintain bone health and overall well-being.

Balanced Diet for Bone Health
While calcium, magnesium, and vitamin D are essential, a well-rounded diet is equally important. Fruits and vegetables provide vitamins, minerals, and antioxidants that support overall health, including bone health. Whole grains offer a source of complex carbohydrates, fiber, and various nutrients that aid in maintaining a healthy weight and preventing inflammation, which can indirectly benefit bone health. Lean proteins, such as poultry, fish, beans, and legumes, are vital for muscle maintenance, and strong muscles are closely tied to strong bones.
Being lactose intolerant can potentially impact bone health as it restricts access to a common source of calcium found in dairy products, which is crucial for maintaining strong bones. Always consult your healthcare professional for advice.
It is well worth looking into the benefits of bone broth, bought or homemade which will support your body through midlife and beyond.

Gut Health
Bone density and gut health are two important aspects of overall well-being. While they may not seem directly related, there is some research suggesting a potential connection between them.
Gut health refers to the balance and functionality of the gastrointestinal tract, including the diverse community of microorganisms (microbiota) that reside in the gut. These microorganisms play a role in digestion, immune system regulation, and even influencing certain metabolic processes.
Research has indicated that there might be a link between gut health and bone density. Some studies suggest that a healthy gut microbiome can contribute to better nutrient absorption, ove vitamin and minerals essential for bone health. Additionally, certain gut bacteria may play a role in modulating inflammation, which can impact bone health.
However, the relationship between gut health and bone density is complex, and more research is needed to fully understand the mechanisms at play. Factors such as diet, exercise, genetics, and overall health also play significant roles in both gut health and bone density.
Physical Activity and Bone Health
Regular physical activity is a cornerstone of maintaining bone health. Weight-bearing exercises, where you support your body weight against gravity, stimulate bone growth and strength. These activities include walking, hiking, dancing, and stair climbing.
Resistance training, involving activities like lifting weights or using resistance bands, promotes muscle and fascia development, which in turn supports bone health. Balance exercises, such as yoga and tai chi, and foot health, help reduce the risk of falls and fractures by improving stability and coordination.
Lifestyle Choices
Making healthy lifestyle choices can significantly impact bone health. Smoking has been linked to lower bone density and a higher risk of fractures. If you smoke, quitting can contribute to better bone health. Similarly, excessive alcohol consumption can weaken bones and increase the risk of fractures. Limiting alcohol intake can help protect bone health and overall well-being.
Weight and Bone Health
Maintaining a healthy weight is closely linked to strong bones. Both being underweight and overweight can impact bone health negatively. Eating disorders such as anorexia and bulimia will weaken bones.
Underweight: Insufficient body weight can lead to lower bone density, increasing the risk of fractures. Inadequate nutrition often accompanies underweight conditions, depriving bones of essential nutrients needed for strength.
Overweight: Excess body weight can strain bones and joints, particularly in weight-bearing areas like the spine, hips, and knees. Additionally, excess fat can produce hormones that trigger inflammation, and withhold Vitamin D from the body potentially affecting bone health.
Striking a balance is key. Aim for a healthy weight through a balanced diet and regular exercise, which can not only benefit bones but also overall well-being. Consulting a healthcare professional can provide personalized guidance on maintaining an optimal weight to support bone health.
Stress Management
Chronic stress can affect hormonal balance, potentially impacting bone health. When stressed, the body produces cortisol, which, in excess, can lead to bone loss. Incorporating stress-reduction techniques into your routine, such as meditation, deep breathing, and mindfulness, can help maintain hormonal balance and support bone health.
[CTA]
Adequate Sleep
Quality sleep creates overall health, and it also plays a role in bone health. During sleep, the body repairs and regenerates tissues, including bone tissue. Aim for 7-9 hours of restful sleep each night to support optimal bone health and overall well-being.
Regular Health Check-ups
Regular check-ups and bone density screenings are essential for early detection and prevention of bone-related issues. If you have concerns about your bone health, discussing them with a healthcare provider can help create a personalized plan to maintain or improve your bone density.
By adopting these natural methods to maintain bone health, women over 45 can take proactive steps to support their overall well-being and enjoy an active and fulfilling life. Remember, it's never too late to prioritize bone health and make positive lifestyle changes that benefit you for years to come.
Your Check List to Bone Health
Finally, prevention lies at the heart of maintaining strong bones and mitigating the risk of osteoporosis. Here is your checklist to seamlessly incorporated into your daily life to bolster bone health:
1. Nourishing Minerals: Prioritize calcium and magnesium-rich foods such as dairy products, or fortified plant-based alternatives, leafy greens, and nuts to provide your bones with essential building blocks.
2. Embrace Vitamin D: Ensure sufficient vitamin D intake through safe sun exposure or dietary sources like fatty fish and fortified products, as it aids in calcium absorption.
3. A Well-Balanced Diet: Opt for a well-rounded diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats to support overall health and bone strength. Include optimal hydration in your well-balanced diet.
4. Stay Physically Active: Engage in regular weight-bearing exercises, resistance training, and balance exercises to fortify bones and muscles.
5. Maintain a Healthy Weight: Strive for a healthy weight through balanced eating and physical activity to reduce strain on bones and joints.
6. Avoid Smoking and Excessive Alcohol: Quit smoking and limit alcohol consumption to safeguard bone health and overall well-being.
7. Manage Stress: Practice stress-reduction techniques like meditation and deep breathing to maintain hormonal balance and promote bone health.
8. Prioritize Quality Sleep: Aim for 7-9 hours of restful sleep each night to facilitate bone tissue repair and regeneration.
9. Cultural Adaptation: Adapt traditional dietary practices to incorporate bone-friendly foods and blend them with modern exercise routines for holistic bone health.
10. Regular Health Check-ups: Schedule regular check-ups and bone density screenings, especially if you're at risk, to monitor bone health and detect issues early.
These tips can serve as effective preventive measures, but it's always advisable to consult a healthcare professional for personalized advice tailored to your individual needs and circumstances. With these strategies in place, you're better equipped to build a solid foundation for lifelong bone health and well-being.